Heart Rhythm 4:200-206, 2007.
other versions
abstract
background Myocardial ischemia causes ST segment elevation or depression in electrocardiograms and epicardial leads. ST depression in epicardium overlying the ischemic zone indicates that the ischemia is nontransmural. However, nontransmural ischemia does not always cause ST depression. Especially in animal models, ST depression is hard to reproduce.
objective The purpose of this study was to determine the circumstances in which ST depression could be expected.
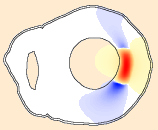
methods We studied ischemia in a large-scale computer model of the human heart. A realistic representation of the ischemia-induced changes in resting membrane potential was used, which was based on diffusion of extracellular potassium. Ischemia diameter, transmural extent, and tissue conductivity were varied.
results Our simulations confirm earlier work showing that partial-thickness ischemia, like full-thickness ischemia, typically causes ST elevation in an anisotropic model of the ventricles. However, we identified three situations in which ST depression can occur in overlying leads. The first is a reduced anisotropy ratio of the intracellular conductivity, which may result from hypertrophy and gap-junctional remodeling, circumstances that are likely to accompany ischemia. Second, an increase of the extracellular anisotropy has the same effect. Third, ST depression was found, independent of the anisotropy ratios, in very large and thin ischemic regions, resembling those that may occur in left-main or multivessel disease.
conclusion Both tissue remodeling and geometric factors can explain ST depression in overlying epicardial leads. We note at the same time that ST elevation is found in most circumstances, while depression occurs as a reciprocal effect, even in partial-thickness ischemia.
lay abstract
The electrocardiogram (ECG) is the first diagnostic test performed on patients with symptoms of heart attack, and often the only test. Treatment and further testing depends on whether they have an upward change of the ST segment in their ECG (ST-elevation myocardial infarction, STEMI) or only downward changes (non-STEMI). The latter group of patients has a lower short-term risk, and does not always require the same urgent treatment as STEMI patients. However, the long-term prognosis is similar for both groups. This suggests that better treatment of non-STEMI patients is possible.
STEMI is almost always caused by an obstruction of a coronary artery, one of the large vessels that provide the blood supply for the heart muscle itself. The traditional view on non-STEMI is that it is simply less severe, and due to a partial obstruction. Using a computer heart model we have shown that this would not explain a negative shift in the ST segment of the ECG. This result indicates that much more is going on in the heart of non-STEMI patients than is often thought.
funding
Computational resources for this work were provided by the Réseau québécois de calcul de haute performance (RQCHP). M. Potse was supported by a postdoctoral research award from the Groupe de recherche en sciences et technologie biomédicale (GRSTB), École Polytechnique and Université de Montréal; and by the Research Center of Sacré-Coeur Hospital, Montréal, Québec, Canada.